After taking time and processing everything that has occurred, I think it’s time to tell our story. On August 1st, I received a phone call while at work from my husband stating that PJ was having severe abdominal pain. Since we’ve been dealing with severe abdominal pain along with other abdominal symptoms X’s 1 year (he has been evaluated several times), this was nothing out of the norm, so I told my husband to give PJ Tylenol & try to see if he could have a BM. He was “diagnosed” on June 24th with “lactose intolerance,” “increased sensitivity to the internal organs,” & “constipation.” The abdominal pain continued to worsen, so we decided to head to the ER.
When we arrived at St. Tammany ER, his temp was 93.8, he was very lethargic, glucose was 408, white count 25,000, and lactic acid 7.1. After an abnormal abdominal X Ray, we went to CT, which showed central mesenteric volvulus or internal hernia with colonic obstruction. They made a quick decision to airlift him to Children’s in New Orleans, but since the weather was terrible, we had to be transported by ambulance.
He needed emergency surgery ASAP! When we arrived at Children’s, his condition worsened. He was very “out of it,” began vomiting, and passed out in the bathroom. After his syncopal episode, they finally got the ball rolling to take him for an emergency ex lap. The 1st surgery showed multiple twisted loops of bowel at the base of the mesentery, midgut volvulus, and internal hernia with long segment dusky discoloration of the long small bowel loop and part of the colon.
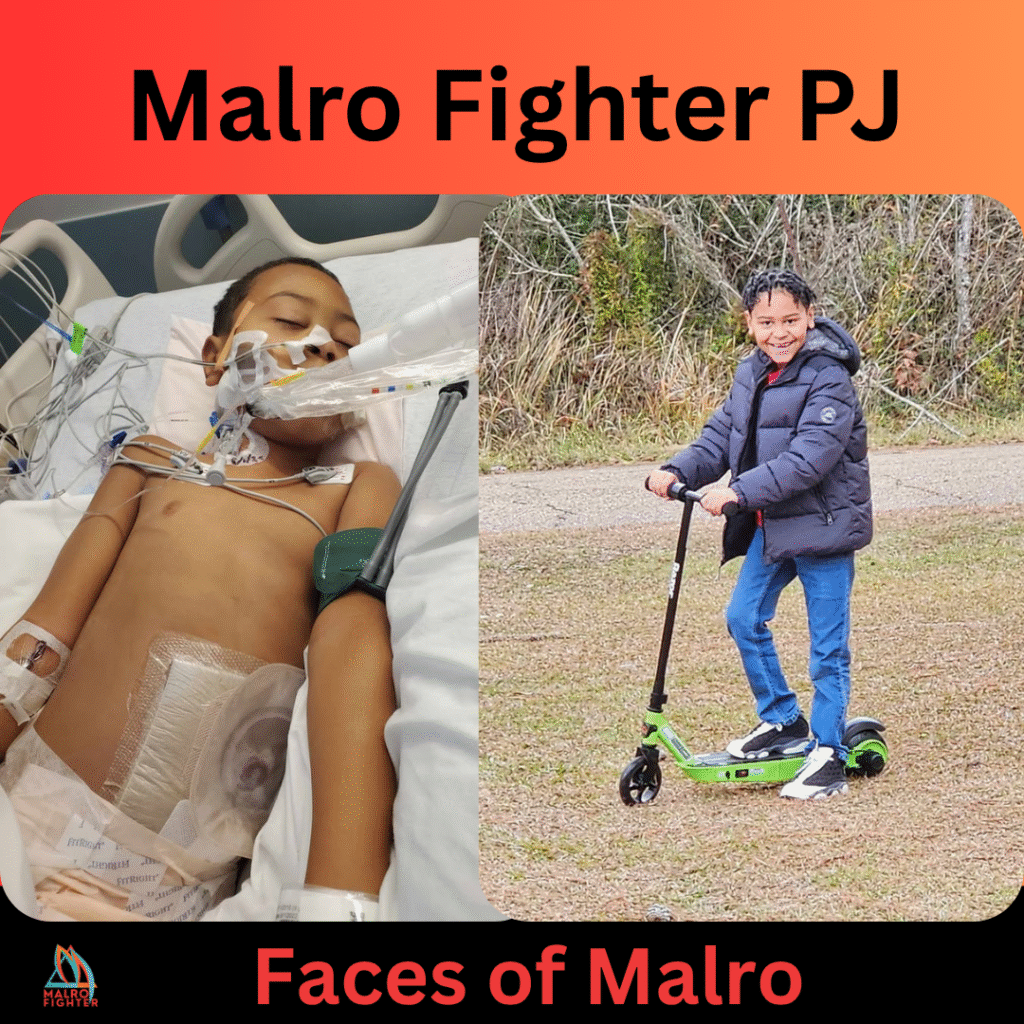
They made the decision to leave him open & go back in the next day to reevaluate. That night was the worst night of our lives. All we were being told was, “He is a very sick little boy.” Our baby was septic! ![]() The next day, he was taken back into surgery and they found the small bowel appeared much more viable than at the first operation, so they decided to reapply abthera and take another look the next day in an attempt to conserve as much bowel as possible.
The next day, he was taken back into surgery and they found the small bowel appeared much more viable than at the first operation, so they decided to reapply abthera and take another look the next day in an attempt to conserve as much bowel as possible.
The following day, he was taken back to surgery with the following findings: 328 centimeters of distal bowel was unsalvageable (63.5% of small bowel)—135 cm of normal-appearing proximal jejunum. The next 45 cm had recovered enough from the ischemia to be viable, but were not completely normal. 8 cm of normal appearing terminal ileum. Normal appearing colon with full recovery of the redundant sigmoid loop. He had a temporary jejunostomy for approximately 2-3 months and was on a ventilator until August 5th.
After improving, he was transferred to the floor, but then he dehydrated very quickly & his potassium levels shot up extremely high. We were brought back to the PICU for the day/night until treatment for those 2 began working and he showed improvement. Then we went to work on decreasing ostomy output, working on hydration, and healing.
He did well until August 25, when he began vomiting and complaining of severe abdominal pain. X-ray & CT show a dilated bowel, and an NG tube was placed. The following day, on August 27th, he was taken to the OR for Broviac Central Line placement & the decision was made to proceed with a 4th ex lap. Thank God prayers were answered & all was normal except inflamed intestines.
After several days of NPO & healing, he began to improve once again. We were then on the road to recovery and going home! A little over a week later, on September 6, 2022, we were cleared for discharge! All of his doctors & surgeons say he is a true miracle! PJ has had a few bumps in the road and hospital admissions in between, but he has done awesome.
He remained on TPN & lipids & home until he became septic again on January 8, 2023, due to central line infection and they decided then to discontinue. He has since begun to do very well and has even gained a few pounds.”







